Payment Posting & Reconciliation



2x Faster Provider Credentialing
Stay Compliant, and Focus on Patient Care
Provider credentialing is a crucial step for healthcare professionals and facilities to get enrolled with insurance networks, hospitals, and regulatory bodies. Without proper credentialing, providers may face claim denials, delayed reimbursements, and restricted patient access.
At Details RCM LLC, we take the complexity out of credentialing by managing the entire process—from application submission to ongoing compliance. Whether you’re an individual provider or a healthcare organization, our expert team ensures a smooth and efficient credentialing experience, so you can focus on delivering quality care without administrative hassles.
What is Provider Credentialing?
Provider credentialing is the essential process of verifying a healthcare provider’s qualifications, experience, and professional background. It ensures that medical professionals meet the necessary standards to work with insurance companies, hospitals, and healthcare organizations.
At Details RCM LLC, we manage this complex process for you, eliminating delays and ensuring full compliance with insurance and regulatory requirements.
Why Choose
Details RCM LLC for RCM?
Credentialing is a complex and time-consuming process that requires attention to detail, compliance expertise, and continuous follow-ups with insurance networks. At Details RCM LLC, we simplify this process, ensuring accuracy, efficiency, and timely approvals. Our dedicated credentialing specialists work closely with providers to help them get enrolled quickly and avoid unnecessary delays.
Fast & Hassle-Free Credentialing
We streamline the entire credentialing process, minimizing paperwork and reducing processing times to get you enrolled faster and affordable.
Compliance & Accuracy
Our experts ensure that all applications meet insurance payers’ requirements, reducing the risk of rejections and compliance issues.
End-to-End Credentialing Support
From initial credentialing to re-credentialing and ongoing maintenance, we handle everything so you can focus on patient care.
Contract Negotiation Expertise
We help providers secure favorable contracts with insurance networks, improving reimbursement rates.
Nationwide Credentialing Services
Whether you are credentialing for a single state or multiple locations, we assist healthcare providers across all 50 states.
Dedicated Credentialing Specialists
Our team provides personalized support, proactive follow-ups, and regular updates to keep you informed.
Get Credentialed Faster – We Handle Everything
Let our experts manage the entire credentialing process, ensuring quick approvals and compliance so you can focus on patient care.
Seamless RCM with Leading Insurance Networks
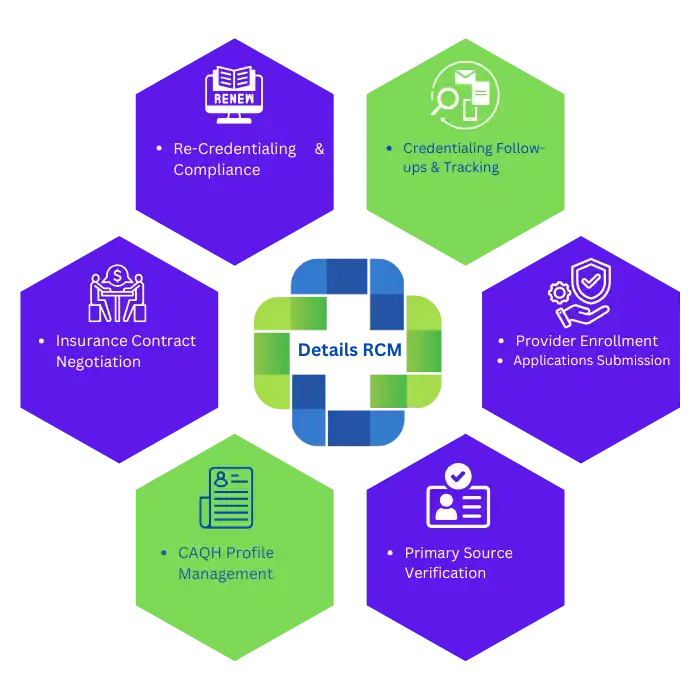
Details RCM offers comprehensive provider credentialing services, ensuring hassle-free enrollment with major insurance companies. We handle the entire credentialing process, including application submission, primary source verification, CAQH profile management, and contract negotiations, helping healthcare providers gain network participation quickly and efficiently.






Why Trust Details RCM for Payment Posting
We make sure every payment is posted correctly and on time, helping your practice maintain steady revenue and avoid unnecessary delays.
1
Specialty Experience
We handle posting for all types of practices, ensuring accuracy across every specialty.
2
Early Error Detection
We catch posting issues early to keep your payments moving without delays.
3
Clear Reports
We provide easy-to-read updates that help you stay informed at every step.
4
Workflow Support
We work alongside your staff to keep your billing process smooth and efficient.
Other RCM Services
In addition to payment posting, Details RCM offers end-to-end revenue cycle support designed to streamline your operations and improve financial outcomes.

patient registration
We ensure fast, accurate patient intake for smooth front-end operations.

Insurance Verification
We verify coverage upfront to reduce claim rejections and billing delays.

Prior Authorization Services
We manage authorizations efficiently, so your team can focus on care.

Medical Billing and Coding
Our certified experts code and bill with precision for faster reimbursements.

Claim Processing
We submit clean claims quickly and follow up to ensure timely payments.

Claims Denial Management
We resolve denials and identify patterns to prevent future issues.

AR Management
We track and manage outstanding balances to optimize your cash flow.

Patient Billing & Collections
Clear communication and patient-friendly billing improve collection rates and satisfaction.

