Provider Credentialing



Get Credentialed.
Get Paid. Stay Compliant.
At DetailsRCM, we streamline the provider credentialing process to ensure your healthcare practice is compliant, contracted, and capable of receiving timely reimbursements. Whether you’re a solo provider or a multi-specialty group practice, our credentialing experts manage every detail, so you don’t have to.
What is Provider Credentialing?
Provider credentialing is the process of verifying a healthcare professional’s qualifications, experience, and professional history to ensure they meet the standards required by insurance networks and regulatory bodies. It is essential for joining payer networks, receiving reimbursements, and maintaining a trustworthy professional standing.
Our Provider Credentialing
Services
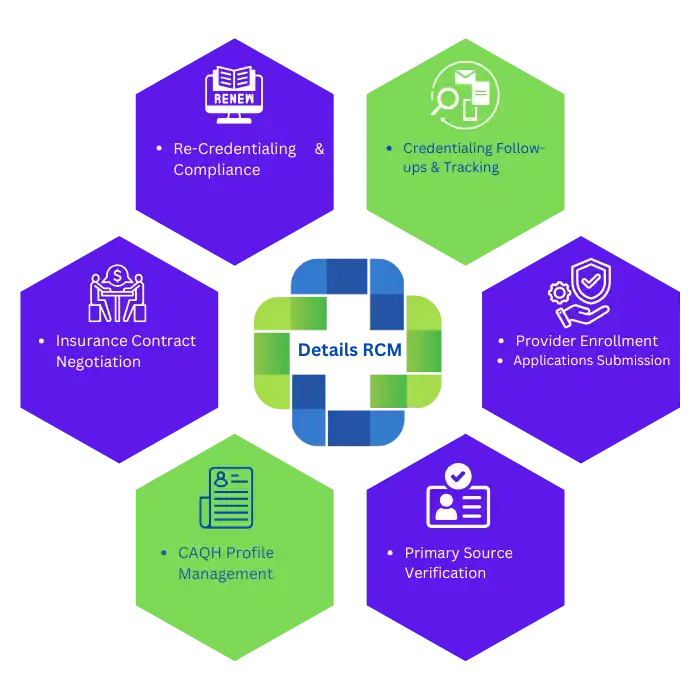
At DetailsRCM, we offer a wide range of provider credentialing solutions tailored to meet the needs of individual practitioners, group practices, and healthcare organizations. Our services ensure that providers are properly enrolled, verified, and maintained within insurance networks—streamlining compliance and accelerating reimbursements.
Initial Provider Credentialing
We help new healthcare providers get credentialed and enrolled with insurance payers, including Medicare, Medicaid, and commercial plans.
- CAQH profile setup and attestation
- NPI registration assistance
- State license and DEA verification
- Payer application submission and tracking
Re-Credentialing & Maintenance
Stay active with payers and avoid credentialing-related payment delays.
- Payer re-credentialing every 2–3 years
- Monitoring license and document expirations
- Timely re-attestation of CAQH profiles
- Ongoing compliance support
Payer Enrollment & Contracting
We handle the enrollment and contracting process to ensure you can accept insurance patients.
- Insurance panel participation applications
- Fee schedule analysis and contracting assistance
- Follow-up and status tracking with payers
- Credentialing status reporting
Contract Negotiation Expertise
Credentialing solutions for group practices and healthcare organizations.
- Group NPI and TIN-based enrollments
- Individual provider additions to group contracts
- Credentialing file management for multiple providers
- Delegated credentialing support (if applicable)
Credentialing File Setup & Management
We create and maintain a digital credentialing file to streamline updates and renewals.
- Centralized documentation storage
- Expiration alerts and reminders
- Credentialing history logs
- Easy access for audits and updates
Credentialing Audit Support
Ensure you’re ready for payer or internal audits with organized and accurate credentialing records.
- Pre-audit credentialing file reviews
- Gap identification and resolution
- Documentation support during audits
- Corrective action planning
Join Insurance Networks
with Ease
Let our experts manage the entire credentialing process, ensuring quick approvals and compliance so you can focus on patient care.
Hustle Free
Provider Paneling With Payers in Every State
Our credentialing experts manage the entire provider credentialing and paneling process from start to finish. We handle all paperwork, ensure regulatory compliance, and follow up with insurance payers on your behalf.
From initial applications to ongoing communication, we streamline your credentialing to help secure faster approvals and in-network participation, so you can focus on delivering quality care while we handle the admin work.






01
Application Submission Process
Gathering and submitting required documents to payers for enrollment.
02
Verification & Credentialing Service
Ensuring provider credentials meet payer requirements through verification.
03
Contract Negotiation
Reviewing and negotiating payer contracts for better reimbursement rates.
04
Approval & Enrollment
Securing final approval and adding providers to payer networks.
How We Work
Who We Assist
With Credentialing
We help a range of medical practitioners with getting their provider credentialing done right and fast.

Nurse Practitioners (NPs)
RNs and Physician Assistants (PAs) run practice providers who diagnose and treat patients.

Physical, Occupational & Speech Therapists
Rehabilitation professionals working in hospitals and private clinics.

Optometrists & Ophthalmologists
Eye care specialists involved in vision correction and surgery.
Frequently Asked
Questions
Find quick answers to the most commonly asked questions about provider credentialing and enrollment.

We Are Here To Help With Your queries !
Provider credentialing is the process of verifying a healthcare provider’s qualifications, licenses, and experience to ensure they meet payer and regulatory requirements.
Credentialing is essential for providers to bill insurance companies, gain hospital privileges, and ensure patient safety and compliance.
The credentialing process typically takes 60 to 90 days, but it can vary depending on the payer and completeness of submitted documents.
Common documents include medical licenses, malpractice insurance, DEA registration, board certifications, and work history.
Yes, credentialing is required for doctors, nurse practitioners, therapists, chiropractors, dentists, and other licensed professionals working with insurance payers.
CAQH ProView is an online database where providers store and update their credentials, making the credentialing process faster and more efficient.
Yes, most payers require re-credentialing every 2-3 years to verify updated provider information and compliance.
In most cases, no—insurance payers require approved credentialing before reimbursement. Some providers may qualify for provisional credentialing in certain states.
Delays can result in lost revenue and unpaid claims. If denied, the provider must correct errors, submit additional documentation, or appeal.
A credentialing service handles paperwork, follows up with payers, ensures accuracy, and reduces processing time, allowing providers to focus on patient care.




