ReCredentialing



Re-Credentialing
& Contracting Made Easy
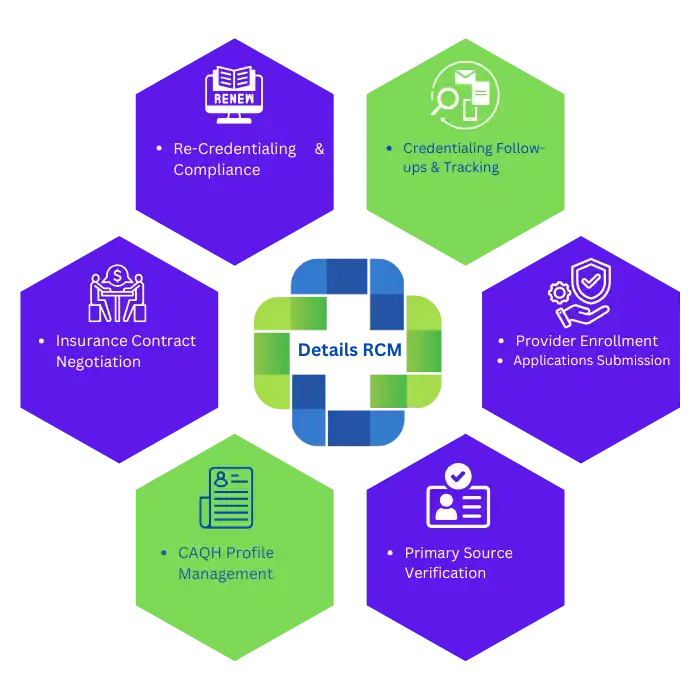
Stay compliant and keep your practice running smoothly with our professional re-credentialing and contracting services. At Details RCM, we manage the entire process — from updating provider credentials to negotiating new contracts with insurance payers. Our experienced team ensures you maintain active participation in insurance networks without delays, helping you avoid payment interruptions and stay focused on patient care. Trust us to handle re-credentialing and payer contracting efficiently, so your revenue never stops flowing.
What is Re-Credentialing?
Re-credentialing is the process of renewing and verifying a healthcare provider’s credentials to maintain participation in insurance networks. Insurance companies require providers to undergo re-credentialing every 2–3 years to ensure their licenses, certifications, and practice details remain accurate and up to date. At Details RCM, we streamline this process to prevent disruptions in payer contracts and reimbursements — keeping your practice compliant and financially secure.
Why Choose
Details RCM LLC for Re-Credentialing
Partner with Details RCM LLC for seamless re-credentialing services that keep your practice compliant and revenue flowing. We handle renewals, verifications, and payer communication—so you don’t have to.
Updated Provider Information
Ensure all personal, licensure, and practice details are current and accurate for payer verification.
License & Certification Verification
Confirm active state medical licenses, board certifications, and DEA registrations are valid and up to date.
Malpractice Insurance Documentation
Submit proof of current malpractice coverage as required by most insurance networks.
Hospital Privileges Confirmation
Verify active hospital affiliations and privileges to maintain network eligibility.
CAQH Profile Maintenance
Keep your CAQH profile updated and attested to streamline payer access and approval.
Timely Submission & Follow-Ups
Submit re-credentialing applications on time and track follow-ups to avoid payment disruptions.
Secure Your Network Participation
Re-Credential with Us
Ensure uninterrupted network participation and avoid payment delays by re-credentialing with us today.
Get In-Network
with Major Insurers Across the U.S.
Staying in-network with major insurance companies is key to avoiding claim denials and revenue loss. At Details RCM, we take the stress out of recredentialing by managing the entire process for you. Our team keeps your CAQH profile current, verifies all necessary documents, and submits your recredentialing applications to top insurance payers nationwide. We ensure your provider status stays active with no delays or missed deadlines. While you focus on delivering quality care, we handle the paperwork and keep your enrollment up to date.






01
Consultation & Info Gathering
We start by understanding your credentialing needs, reviewing your current information, and collecting necessary documentation.
02
Application Submission
We handle the submission of re-credentialing applications and set up or update your CAQH profile to ensure accuracy.
03
Verification & Compliance
Our team performs primary source verification and ensures all compliance requirements are met for insurance networks.
04
Follow-Up & Approval
We manage follow-ups with payers, ensuring timely approvals and maintaining your active participation in insurance networks.
Get Started Today
Other credentialing Services
We offer a full range of credentialing solutions to help healthcare providers stay compliant and connected with payers. Whether you’re applying for the first time, updating your CAQH profile, or renewing contracts, our team handles every step with accuracy and speed. Let us simplify the credentialing process so you can focus on delivering care.

Provider Credentialing
We help you get credentialed with insurance companies fast. Our team handles the paperwork and follows up to avoid delays.

CAQH Credentialing
We set up and manage your CAQH profile. Stay compliant and visible to insurance payers without the stress.

Insurance Credentialing
Get enrolled with top insurance networks. We simplify the process so you can start seeing patients sooner.

Medicare & Medicaid Enrollment
We guide you through state and federal program enrollment. Avoid rejections and get approved faster.

ReCredentialing and Contracting
We track expiration dates and handle recredentialing before deadlines. Stay active with your payers without interruptions.

Hospital Privileging
Need hospital access? We prepare and submit all forms for hospital privileges and medical staff appointments.
Frequently Asked
Questions
Find quick answers to the most commonly asked questions about provider credentialing and enrollment.

We Are Here To Help With Your queries !
Re-credentialing is the process of renewing a provider’s credentials to keep working with insurance networks.
It keeps you in-network, ensures your info is up to date, and avoids payment delays.
Most insurance plans require re-credentialing every 3 years. Some may ask sooner.
Start 4–6 months before your current credentialing expires to avoid any coverage gaps.
You’ll need updated licenses, malpractice insurance, work history, and a current CAQH profile.
You could be removed from insurance panels and must stop billing until you’re re-approved.
Yes. You can fix or add new details like licenses or certifications during the process.
It usually takes 30–90 days, depending on how complete your application is.
Yes, if submitted on time. But if you delay, your status might be paused.
An RCM service like Details RCM can manage your paperwork, deadlines, and follow-ups for you.

